Deep Vein Thrombosis Thrombosis is the formation of a blood clot (thrombus), which can partially…

Congestive Heart Failure
Congestive heart failure develops when the heart is weakened and is no longer able to pump an adequate supply of blood to the lungs and other body tissues. Heart failure does not mean that the heart stops pumping, but that it is not pumping efficiently. A number of disorders can lead to heart failure, including heart disease, heart attack, high blood pressure, heart valve disorders, arrhythmias (irregular heartbeats), anemia (a condition in which the oxygen content in the blood is reduced), or cardiomyopathy (a degenerative disease of the heart muscle). Heart failure can occur when the heart muscle is not able to contract effectively (called systolic, or left-sided heart failure) or when the heart muscle is not able to relax (called diastolic, or right-sided heart failure). Other risk factors include smoking, a poor cholesterol profile, high blood pressure, and being overweight.
Heart failure occurs more frequently in men than in women and is twice as common among blacks as among whites. The risk of developing the condition increases with age.
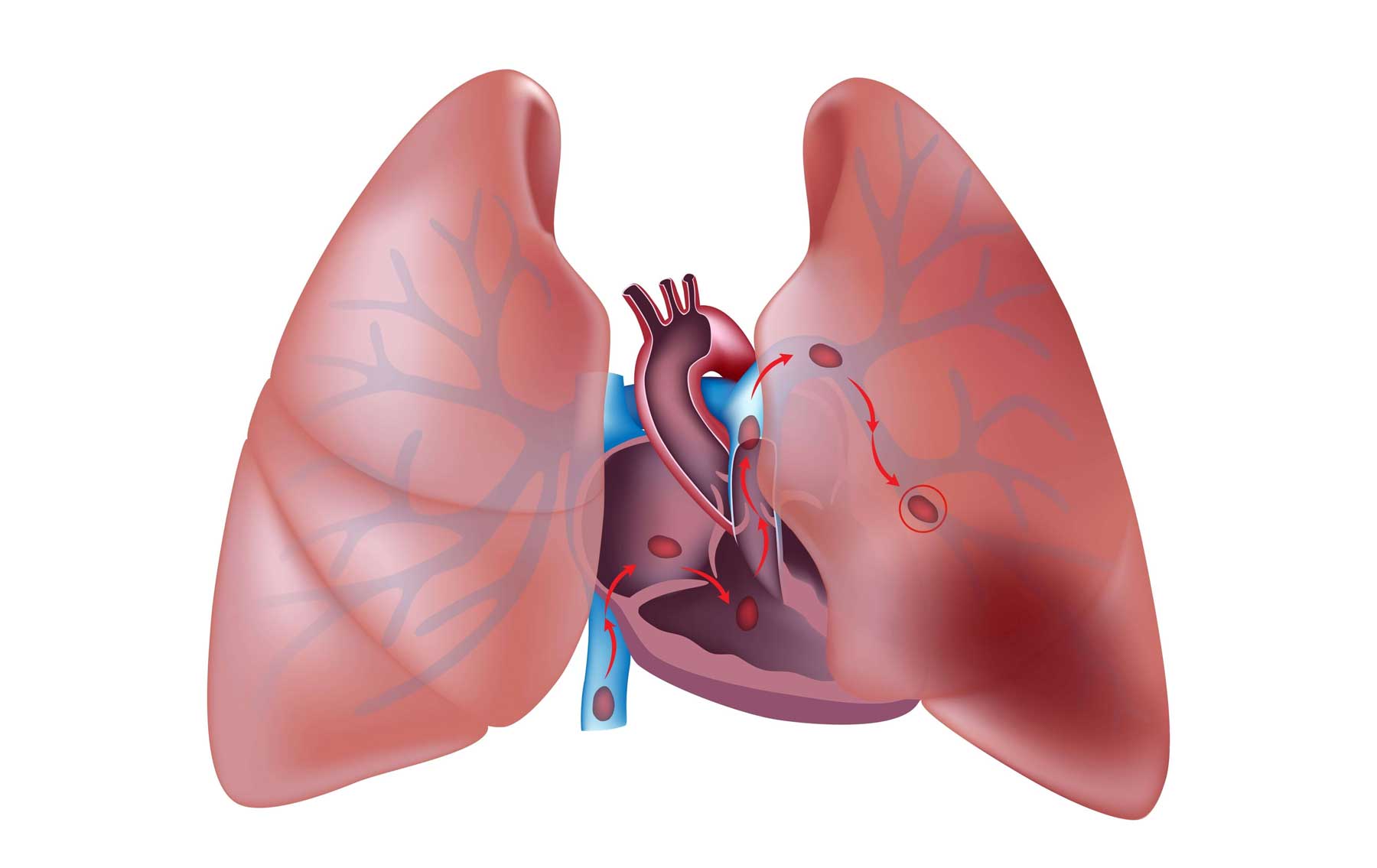
In systolic heart failure, blood backs up in the veins that carry blood from the lungs to the heart, increasing blood pressure in the lungs. The lungs become swollen and congested with fluid. This condition is called pulmonary edema. In diastolic heart failure, blood accumulates in the veins that lead to the heart from other parts of the body. These parts of the body, especially the legs, ankles, and feet, may become swollen. Some people who have diastolic heart failure also have lung congestion.
Despite its name, heart failure is not always life-threatening. The outcome depends on the severity of the underlying disorder that is causing heart failure and on how soon treatment begins. Although there is no cure for heart failure, it can be controlled with medication and a healthy lifestyle.
Symptoms
Heart failure usually develops slowly. The main symptom of heart failure is shortness of breath as a result of lung congestion. You may become short of breath while active or while resting. You may have difficulty breathing when you lie down, and your breathing problems may become severe enough to disturb your sleep. At times you may wake up gasping for air. Although episodes of severe shortness of breath usually last less than an hour, the experience can be frightening.
Your lungs may become so swollen and congested that your breathing may be raspy or you may wheeze. You may also have chest pain and a persistent cough that produces frothy, blood-flecked phlegm. The fluid in your lungs decreases your resistance to infection; pneumonia, for example, is a frequent complication of heart failure.
Fatigue is another common symptom of heart failure. Because your body tissues are not receiving enough oxygen and nutrients, you may feel weak or tire easily. Fluid accumulation may cause the lowest part of your body to swell. For example, if you are confined to bed, the lower part of your back may become swollen. If you are standing, your legs, ankles, or feet may become swollen. Your liver may also become swollen, causing abdominal pain.
Other possible symptoms of congestive heart failure include low blood pressure, dizziness, and confusion. You also may lose your appetite but experience rapid weight gain from the accumulation of fluid.
For some people, symptoms may not develop until the condition is at an advanced stage. The heart muscle attempts to compensate for its decreased pumping ability by growing larger and thicker and contracting more often. However, the effects of this adjustment are only temporary, and symptoms develop eventually.
Treatments
Treatment of congestive heart failure focuses on the underlying disease or condition that is causing it. Your doctor will recommend lifestyle changes you will need to make to improve the quality of your life and control your risk factors for heart disease. For example, if you smoke, your doctor will recommend that you quit smoking. He or she also will recommend that you lose weight if necessary and reduce the amount of fat in your diet. Your doctor also may recommend reducing your intake of caffeine and sodium and eating smaller, more frequent meals, which can help keep you from overeating and can improve your body’s absorption of nutrients. Caffeine can temporarily raise blood pressure and heart rate. For some people, consuming large amounts of sodium (more than 2,400 milligrams a day) can lead to fluid retention, which can increase blood pressure. If you have severe heart failure, you may need to limit your fluid intake to avoid fluid retention. Your doctor will probably recommend that you begin a program of regular, moderate exercise under his or her supervision.
Your doctor is likely to prescribe medication to help relieve your symptoms. Diuretic drugs will help your body eliminate excess fluid and sodium, thereby decreasing blood volume and lowering your blood pressure. Because diuretic drugs increase the body’s output of urine, always take them in the morning to avoid having to get up during the night to urinate.
Other medications frequently prescribed to treat heart failure include digitalis drugs (usually digoxin) and vasodilators such as ACE (angiotensin-converting enzyme) inhibitors. Digitalis drugs slow the heart rate while increasing the strength of the heartbeat and the heart’s output of blood. ACE inhibitors widen both small arteries and veins and counteract some of the substances produced by the kidneys that can narrow small arteries and cause the body to retain fluid. ACE inhibitors reduce the heart’s workload and significantly prolong life in many people. They are powerful drugs, and you and your doctor may need to work together to find the appropriate dosage for you. If you cannot take ACE inhibitors, your doctor may prescribe a nitrate drug or hydralazine, both of which relax smooth muscle to widen blood vessels and improve blood flow. Doctors often prescribe beta blockers to treat heart failure. Like ACE inhibitors, they can relieve symptoms and prolong life in people who have heart failure.
If your doctor prescribes a long period of bed rest, he or she may also prescribe an anticoagulant medication to help prevent the formation of blood clots. If your doctor prescribes an anticoagulant, he or she will carefully monitor the effect of the drug in your blood to help prevent possible complications such as bleeding in the intestines, skin, brain, or other organs.
Drug treatment should relieve your shortness of breath and swelling. By following a low-sodium diet and taking your medication as prescribed, you can expect to lead an active life. However, if your heart failure does not respond to treatment with rest, lifestyle changes, and medication, you may need to have a heart transplant. Heart transplantation has a high success rate. However, because of a severe shortage of donor hearts, the availability of this option is limited. Most people who need a heart transplant are placed on a waiting list until a donor heart becomes available.
Left ventricular assist device
A left ventricular assist device consists of an air-driven pump, a control mechanism, a power source, and connective tubing. The pump and tubing are surgically implanted in the body and attached to the heart. The control mechanism and power source are worn outside the body and are connected by wires to the pump. A tube inserted into the left ventricle draws blood into the pump (inflow). The blood is then pumped out to the tissues through a tube inserted into the aorta (outflow).
Heart transplants
The first human heart transplant was performed in 1967. Since that time, the procedure has become an established treatment for advanced heart disease. Surgeons perform nearly 2,300 heart transplants nationwide each year. Doctors usually recommend a heart transplant only when a person has irreversible, long-term heart failure that cannot be controlled with other medical or surgical treatments. (The artificial hearts now available are still experimental and cannot offer a reliable, long-term solution to the problem of a diseased heart.) Heart transplants can be performed at any age, including infancy and childhood, but the procedure is usually not recommended for people over age 65. The most common causes of heart failure are:
-
- Coronary artery disease (blockage in the arteries leading to the heart)
- Cardiomyopathy (weakness of the heart muscle, affecting its ability to pump blood)
- Heart disease that is present at birth
- Damage to the heart muscle or valves
- Failure of an earlier transplant
After surgery, early symptoms of rejection of the donor heart are not always apparent, so doctors must regularly take tiny samples of the heart muscle and examine them under a microscope (a procedure called a biopsy) to check for signs of rejection. To obtain samples of the tissue, a doctor inserts a small tube into an incision in the neck, down the jugular vein, and into the heart. If the doctor finds signs of rejection, he or she will give the person higher doses of immune-suppressing drugs.
After the person goes home from the hospital for recovery, he or she will have to visit the doctor for regular follow-up visits and more biopsies. Some of the early complications (in addition to rejection) that can arise after heart transplant surgery include kidney failure (which is usually temporary), wound infection, pneumonia, and stroke. Irregular heartbeats called arrhythmias sometimes occur.
Heart transplants now have a high success rate: about 85 percent of those who receive a new heart are alive after 1 year, 79 percent after 3 years, and 74 percent after 5 years. These survival rates continue to improve. Without this lifesaving procedure, the vast majority of heart transplant recipients would have died within 2 years.