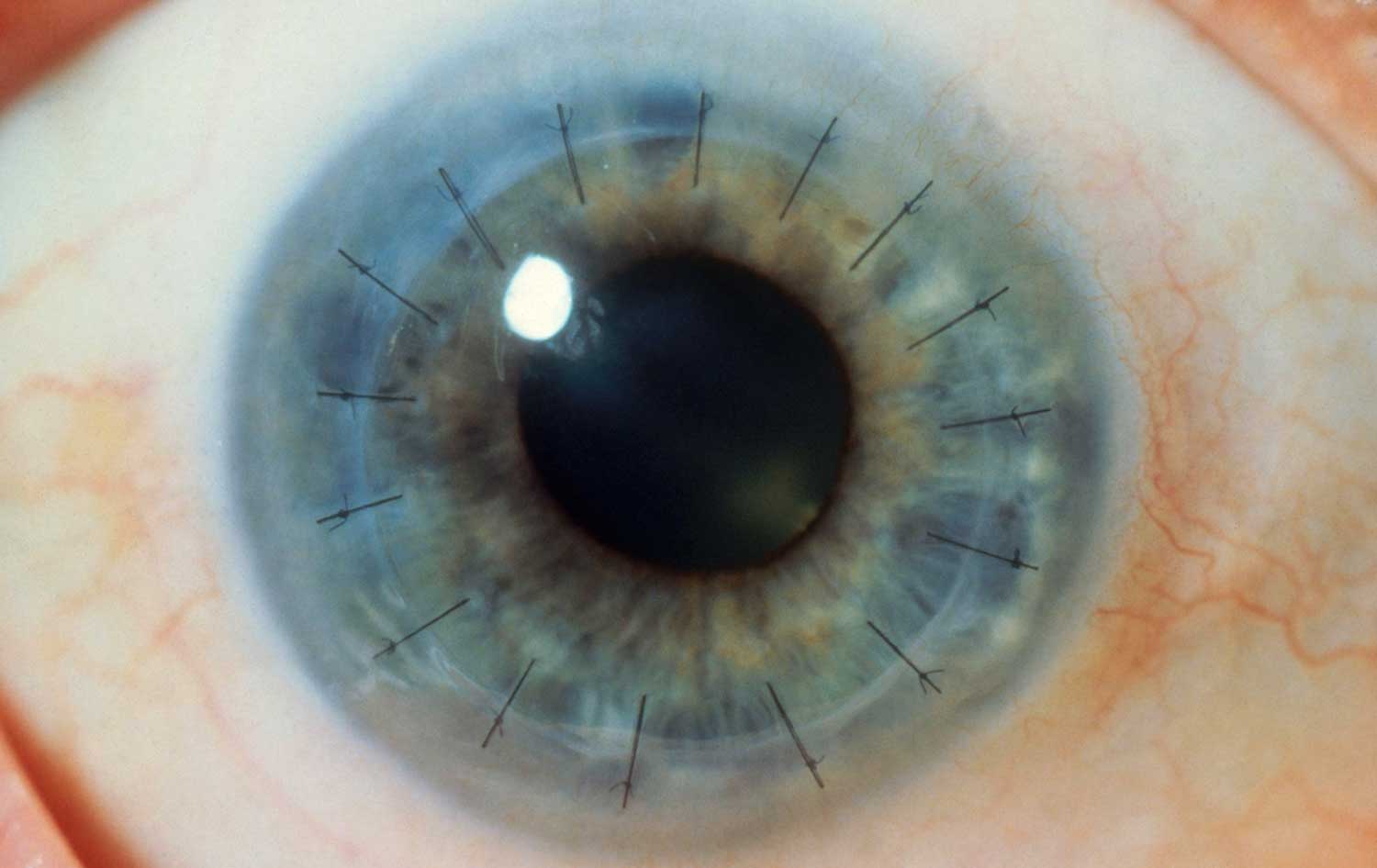
Corneal Transplant Surgery in Iran A corneal transplant, also called keratoplasty replaces diseased or scarred…
Since the outside of the eye is in direct contact with the environment, it is susceptible to infections and injuries. There are also a number of hereditary diseases which can impact the outer eye.
Treatment
Subconjunctival Hemorrhage
July 10, 2021
A subconjunctival hemorrhage is leaking of blood from a small blood vessel in the eye…
Dry eye syndrome
July 8, 2021
Dry eye is a condition that results from inadequate tear production. Although dry eye often…
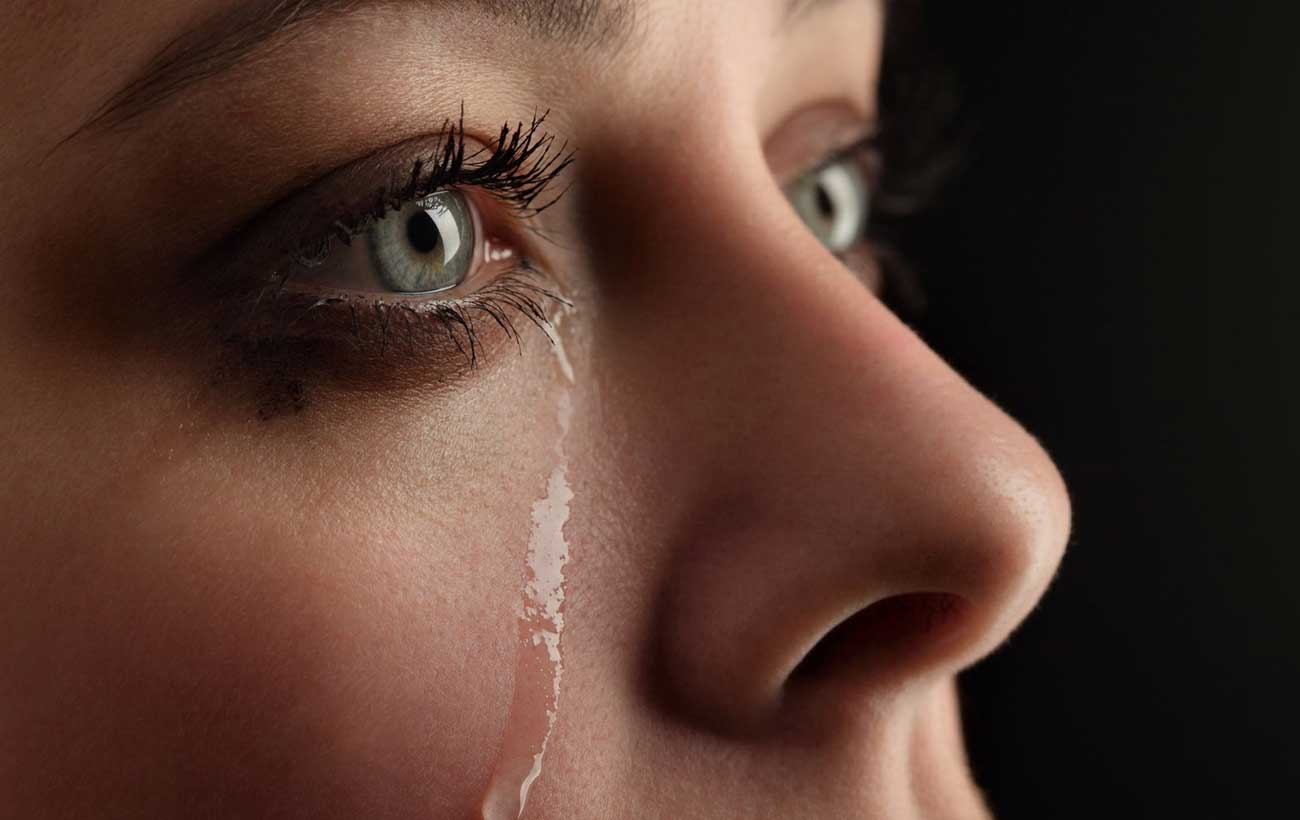
Watering Eye
July 13, 2021
A watering eye is an uncommon condition characterized by continuous tearing of the eye. Sometimes…
Uveitis
July 12, 2021
Uveitis is inflammation of the uvea, which consists of the iris (the colored part of…
Scleritis
July 12, 2021
Scleritis is inflammation of the sclera (the white of the eye). The condition is rare…
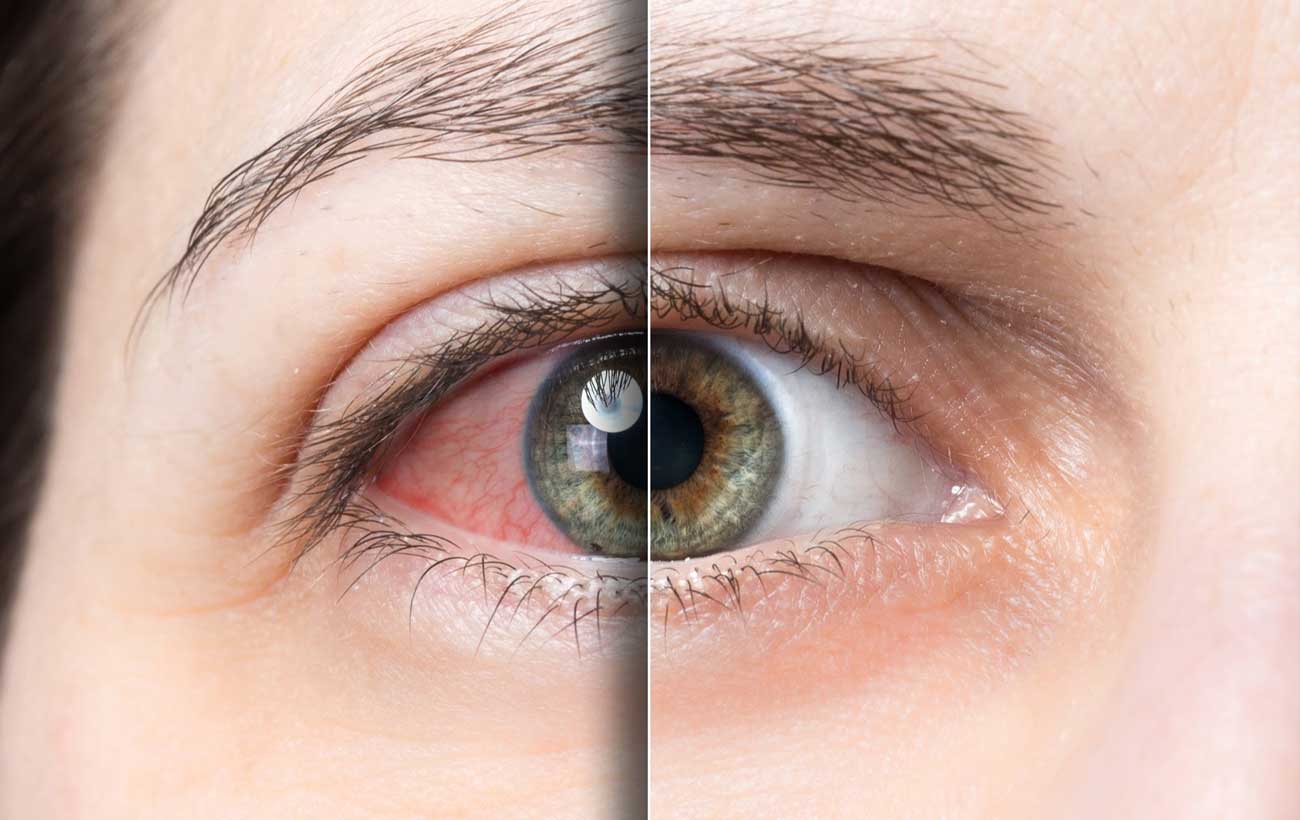
Conjunctivitis
July 10, 2021
Conjunctivitis (also called pinkeye) is inflammation of the conjunctiva, the transparent membrane that covers the…
Best Docotrs