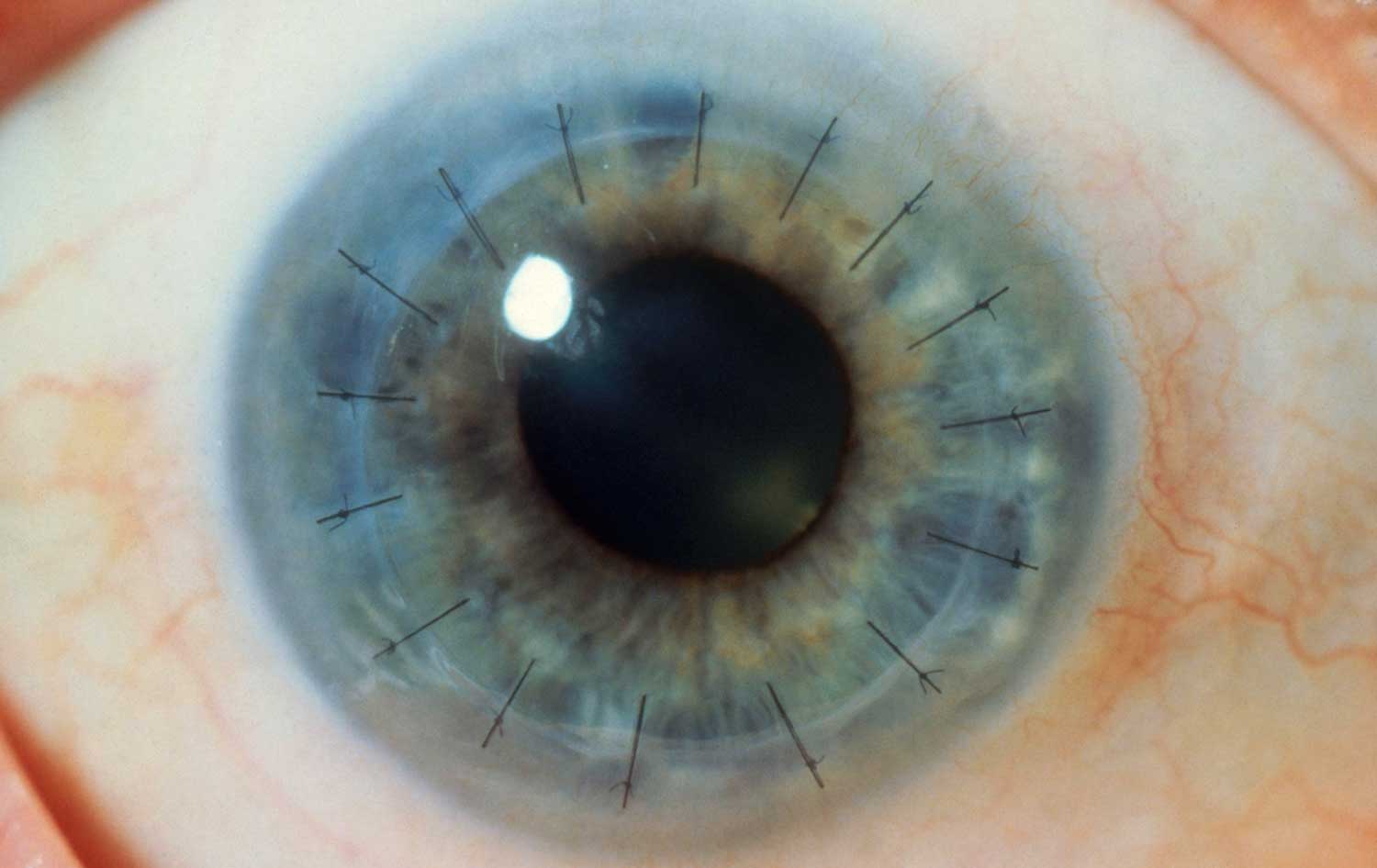
Corneal Transplant Surgery in Iran A corneal transplant, also called keratoplasty replaces diseased or scarred…

Eyelid problems range from benign, self-resolving processes to malignant, possibly metastatic, tumors. Fortunately, most eyelid disorders are not vision-threatening or life-threatening; however, many cause irritative symptoms such as burning, foreign-body sensation or pain.
Ptosis [h3]
Ptosis is a condition in which the upper eyelid droops and partially or completely covers the eye. Ptosis may be congenital (present from birth) and can run in families. However, it also can occur in anyone at any age if the nerve that controls the eyelid muscle or the muscle itself is damaged. The nerve can be damaged by an injury, an underlying disease such as diabetes, or a brain tumor. The muscle can be weakened as a result of muscular dystrophy or myasthenia gravis or as a natural result of aging. Ptosis may affect one or both eyes and may vary in severity over the course of each day.
Treatments [h4]
Ptosis usually improves after successful treatment of any underlying disease. In people whose vision is impaired as a result of ptosis, surgery can be performed to raise the drooping eyelid.
Stye [h3]
Like all hairs, eyelashes grow from tiny pits in the skin called follicles. When a follicle on the eyelid becomes infected, a swelling called a stye develops on the edge of the eyelid around the base of the eyelash.
Treatments [h4]
To help a stye drain earlier, apply frequent warm, moist compresses as soon as it appears, to help draw the pus to a head. Do not squeeze the stye—allow it to open and release the pus on its own. Afterward, wash the eyelid carefully with mild soap or baby shampoo, using a clean, soft washcloth to remove all of the pus. Be careful not to spread the infection.
If a stye does not clear up in a week or so, if the swelling, redness, or tenderness spreads, or if a stye recurs, see your doctor. He or she will examine you, perform tests to determine what type of bacterium is causing the infection, and prescribe an antibiotic to treat the infection.
Chalazion [h3]
A chalazion is a painless swelling on the edge of the eyelid that results from inflammation of one of the meibomian glands, which lubricate the edge of the eyelid.
Treatments [h4]
Chalazions may be small or may grow large enough to cause blurred vision. Although small chalazions usually go away on their own within a month or two, you can speed the process by applying frequent warm, moist compresses to the affected area. For larger chalazions or chalazions that have become infected, a doctor may prescribe antibiotics, corticosteroid eyedrops, or surgery. To remove a chalazion, the doctor administers a local anesthetic, makes a small incision in the eyelid, and scrapes out the contents of the chalazion.
Papilloma [h3]
A papilloma is a slow-growing, benign (noncancerous) skin growth that can develop anywhere on the eyelid.
Treatments [h4]
The color of a papilloma can range from pink to skin-toned. Although a small, inconspicuous papilloma does not need treatment, a doctor may recommend surgery to remove a large, unsightly papilloma. Surgery is usually performed using local anesthesia in a doctor’s office or in an outpatient facility.
Xanthelasma [h3]
In xanthelasma, yellow patches of fatty material (called xanthomas) accumulate beneath the skin of the eyelids, especially near the nose. Xanthelasma usually occurs in older people and is often associated with elevated levels of cholesterol (a fatlike substance in the blood) and triglycerides (the main type of fat in the blood).
Treatments [h4]
Unsightly patches of xanthelasma can be removed surgically. However, they frequently recur, especially if a person’s triglyceride and cholesterol levels remain high.
Entropion [h3]
In entropion, the edge of the eyelid—usually the lower lid—turns inward toward the eye, causing the eyelid and eyelashes to rub against the surface of the eyeball. This continuous rubbing causes the eye to become inflamed and can damage the conjunctiva (the transparent membrane that covers the white of the eye and lines the eyelids) and cornea (the clear, protective covering at the front of the eye).
Entropion usually affects older people. As people age, the fibrous tissue on the lower eyelid loosens, allowing the muscle in the edge of the eyelid to contract abnormally and pull the edge of the eyelid in toward the eye. In some cases, an injury causes scarring on the inner surface of the eyelid, which can pull the edge of the eyelid in.
Treatments [h4]
If the lower eyelid is turned inward, the doctor may recommend turning the eyelid outward to its normal position and holding it there for a few days by attaching one end of a piece of adhesive tape to the eyelid (below the eyelashes) and the other end to the cheek. In some cases, this corrects the condition. The doctor may prescribe eyedrops or ointments to help relieve the pain and inflammation. If entropion persists, an ophthalmologist may recommend surgery to turn the eyelid outward and prevent it from rubbing on the surface of the eyeball. The procedure is usually performed using local anesthesia in a doctor’s office or in an outpatient facility.
Ectropion [h3]
In ectropion, the edge of the eyelid is turned outward and downward away from the eyeball, causing the surface of the eye and the lining of the eyelid to become dry and inflamed. The abnormal position of the eyelid interferes with normal drainage of tears from the eye, causing them to run down the cheek. Losing tears this way can lead to inadequate lubrication of the eyeball, which can damage the cornea (the clear, protective covering at the front of the eye).
Ectropion usually occurs in older people, when aging stretches the tendons of the muscle in the lower eyelid that keep the eyelid snug against the eyeball. The condition can also occur at any age if a scar that has formed on the lower eyelid or cheek tightens or contracts, pulling the eyelid down. If ectropion is not treated, the cornea may be damaged and corneal ulcers may form.
Treatments [h4]
Because ectropion rarely goes away on its own, the doctor will probably recommend surgery to tighten the lower eyelid and move it back to its normal position beneath the eye. The procedure is usually performed using local anesthesia in a doctor’s office or in an outpatient facility.
Blepharitis [h3]
Blepharitis is inflammation of the eyelids. The disorder occurs more often in people who have dandruff, oily skin, dry eye, rosacea, or seborrheic dermatitis. In some cases, a bacterial infection develops and makes the condition worse. Often, flakes from the eyelids enter the eye and cause an inflammatory condition called conjunctivitis.
In severe cases of blepharitis, small ulcers may develop on the edges of the eyelids and, in rare cases, the eyelashes may fall out. Persistent inflammation can lead to the development of corneal ulcers.
Treatments [h4]
To treat blepharitis, a doctor may recommend gently washing away the scaly flakes (morning and night) with a clean, soft washcloth moistened with a solution of warm water and mild, diluted baby shampoo. Rinse the affected area with warm water and pat it dry with a clean, soft towel. If the condition does not improve within 2 weeks, the doctor may prescribe an antibiotic ointment to rub into the edges of the eyelids after washing. He or she may also prescribe eyedrops containing a corticosteroid drug to relieve inflammation. Blepharitis often recurs after treatment.