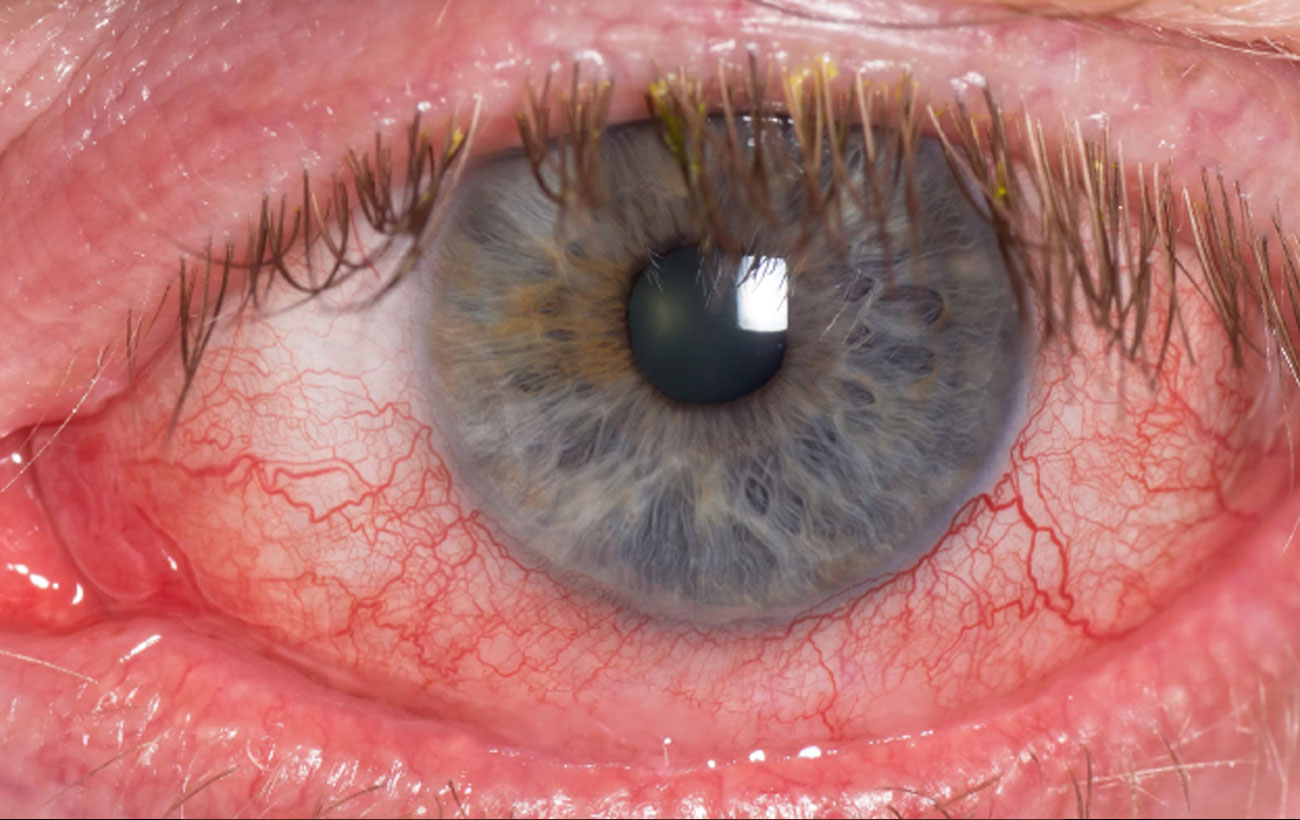
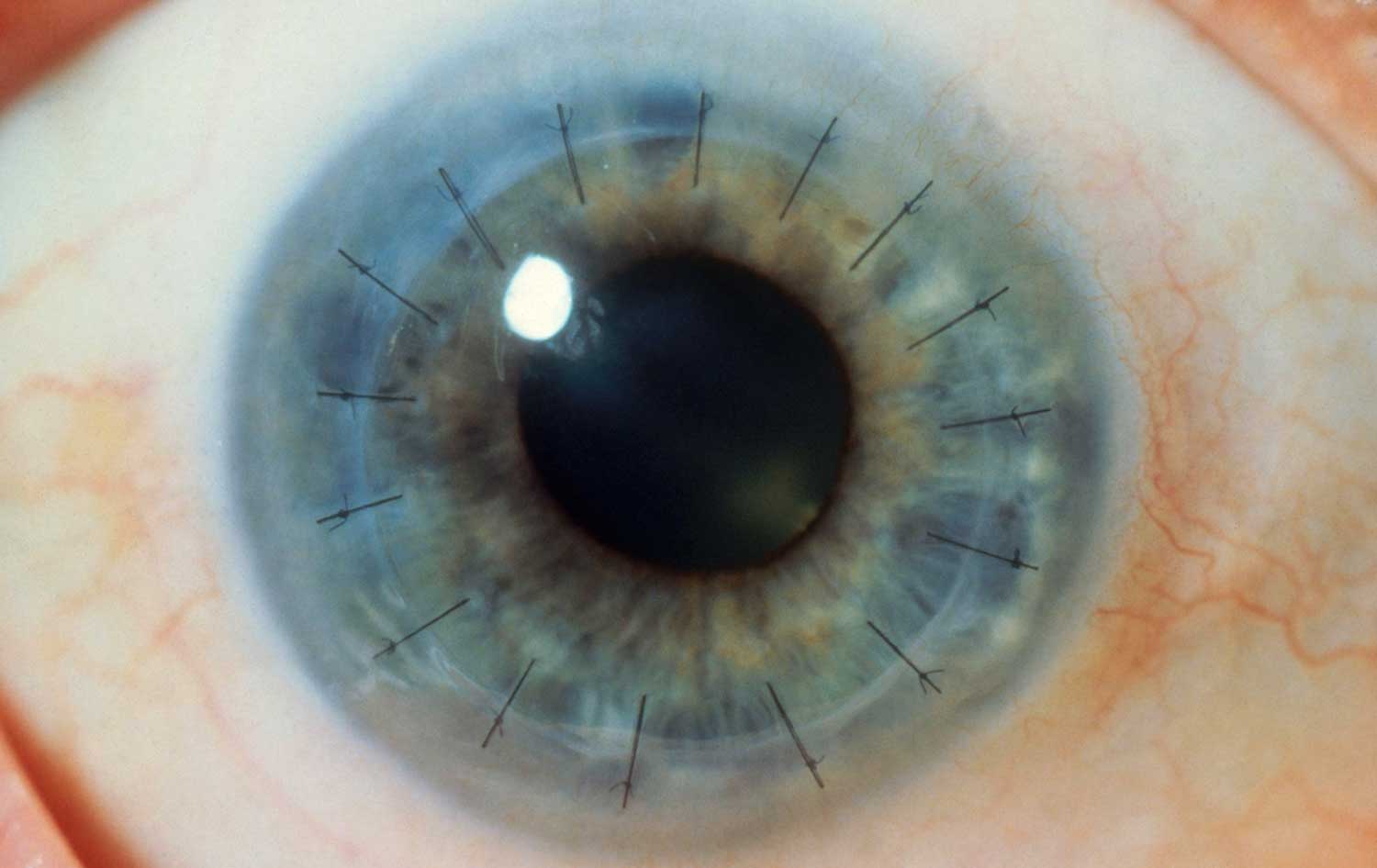
Corneal Transplant Surgery in Iran A corneal transplant, also called keratoplasty replaces diseased or scarred…
Many eye diseases have no early symptoms. They may be painless, and you may see no change in your vision until the disease has become quite advanced.
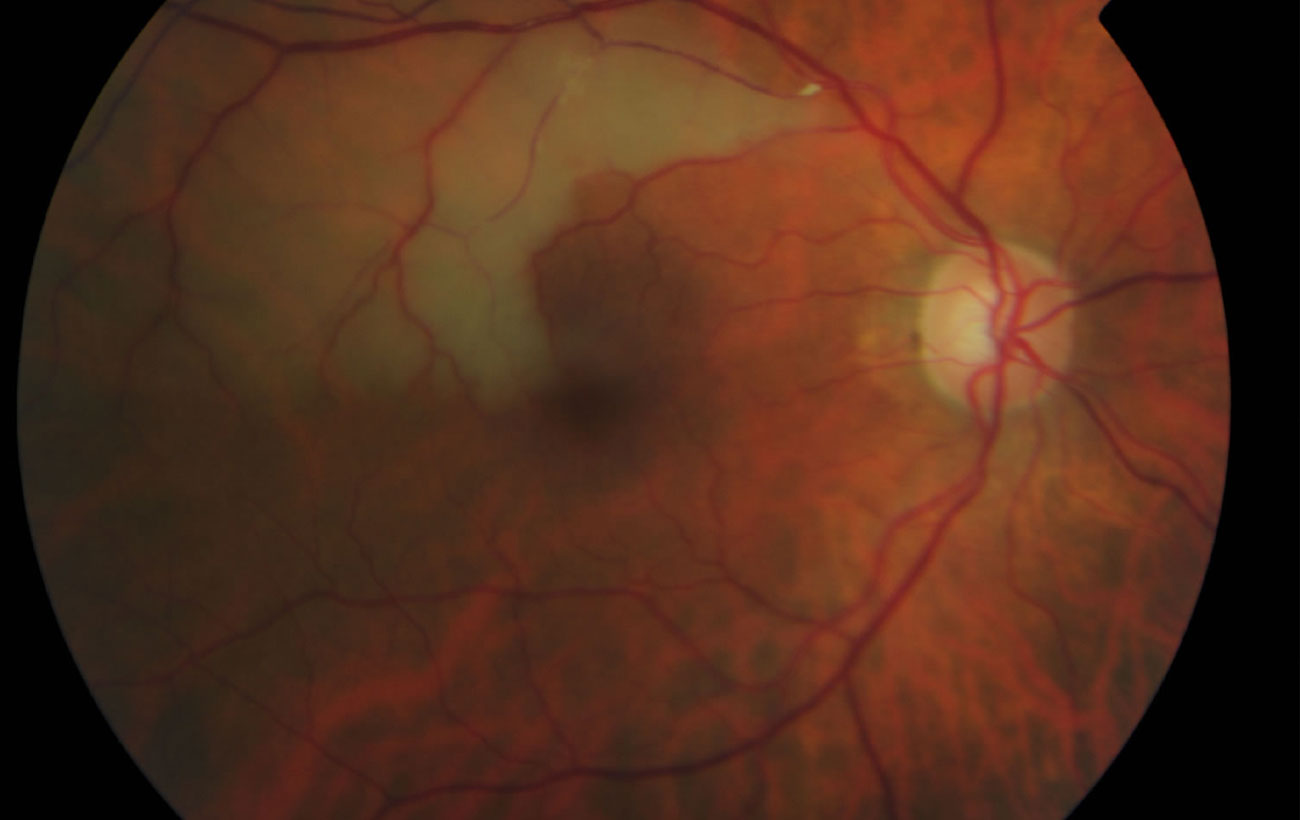
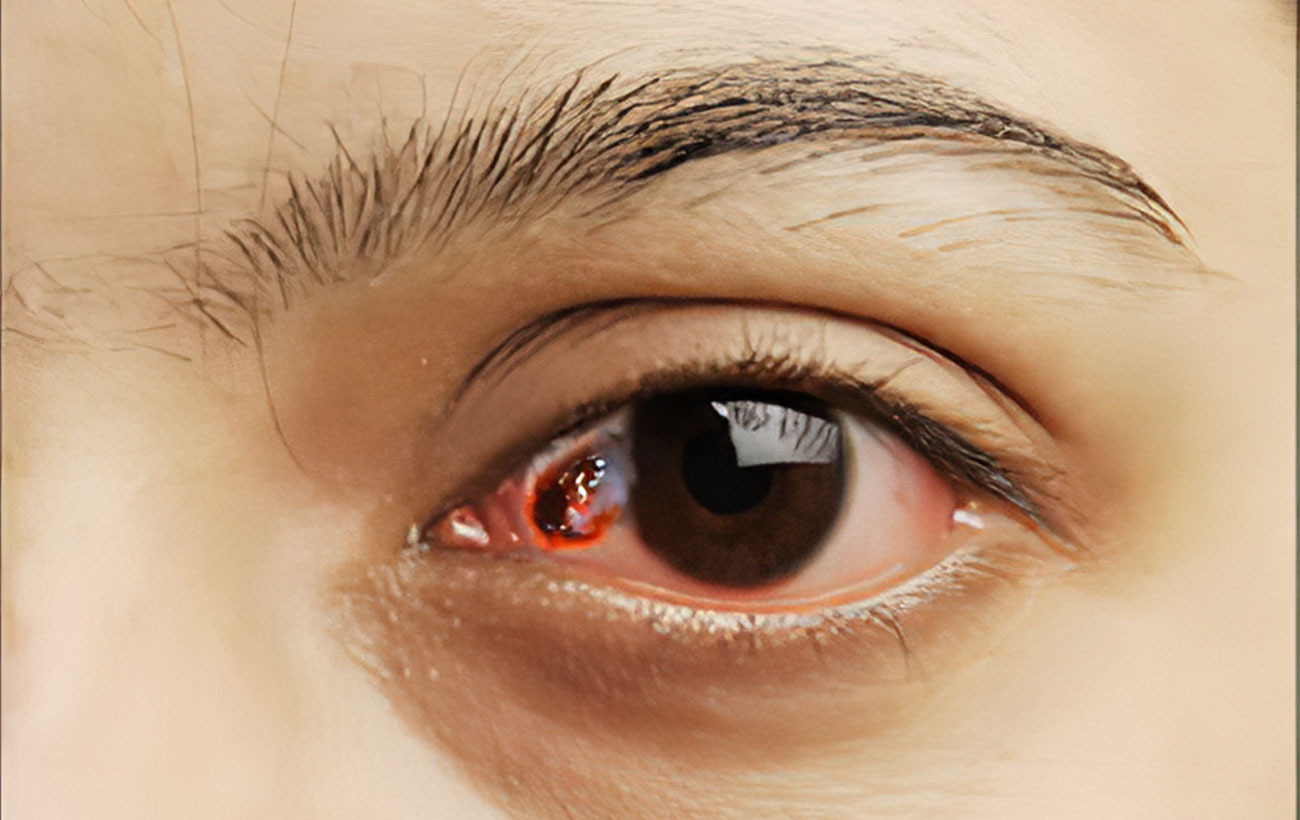
Retinal Artery Occlusion
The retina (the light-sensitive membrane lining the back of the eye) receives…
Macular degeneration
Macular degeneration is a disease characterized by irreversible deterioration of the light-sensitive…
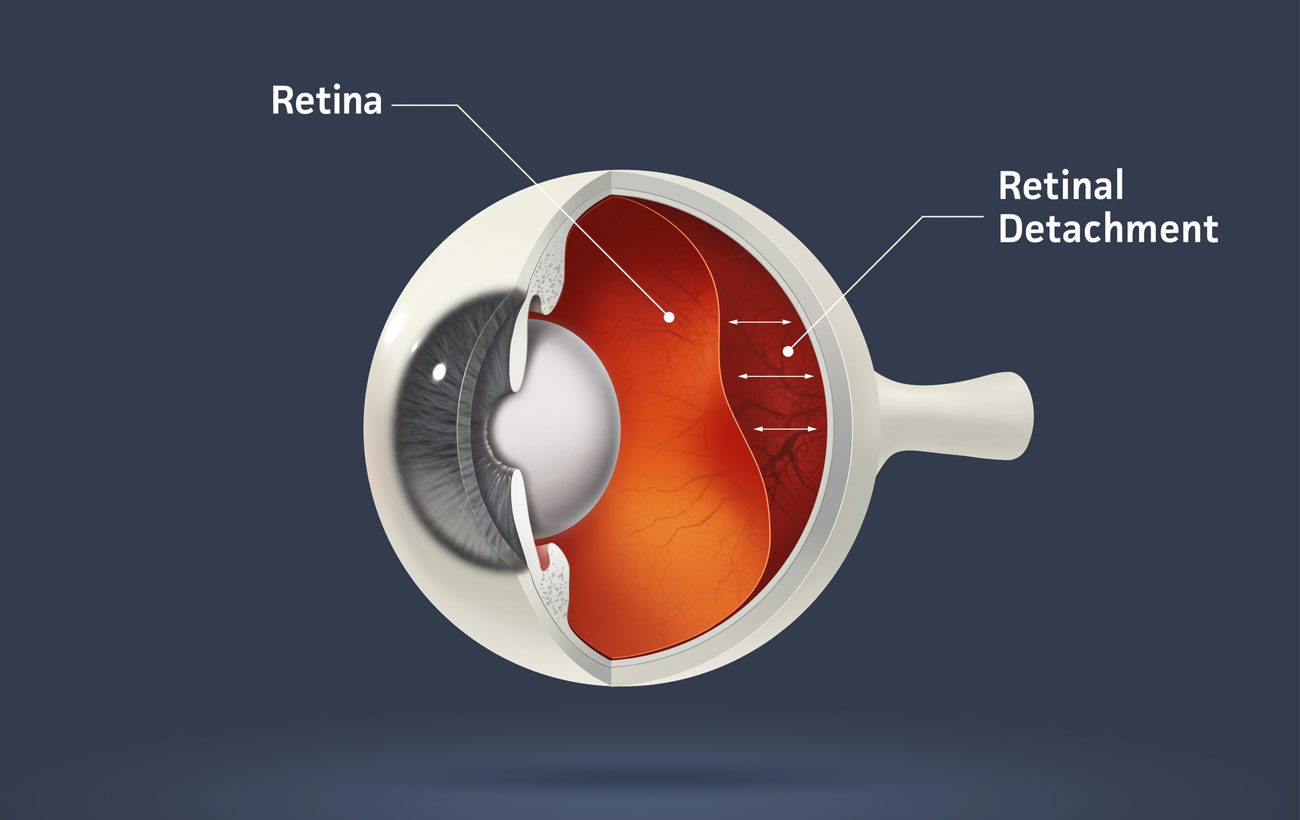
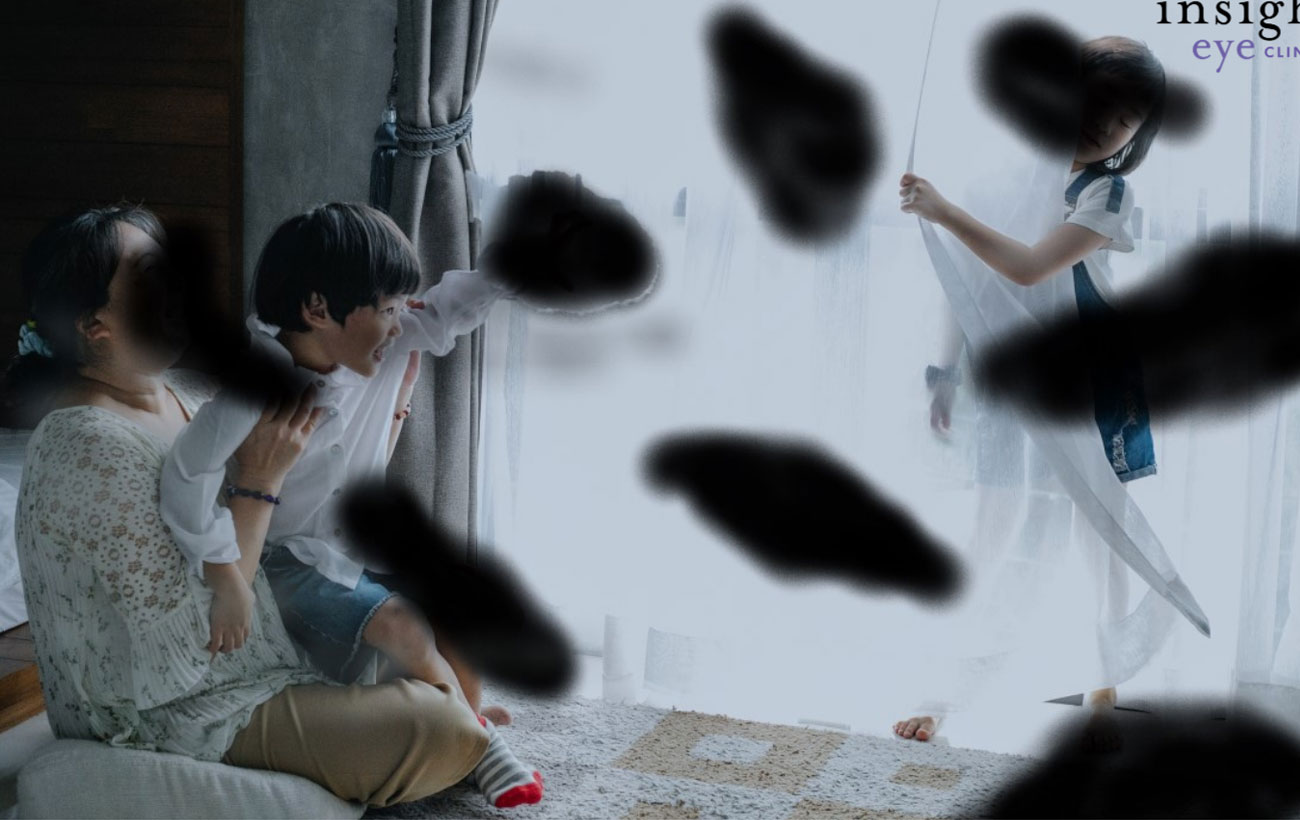
Retinal Detachment
Retinal detachment occurs when the retina—the light-sensitive membrane that lines the inside…
Color Vision Deficiency
Color vision deficiency (also called color blindness) is a vision disorder in…
Retinal Vein Occlusion
The central retinal vein carries oxygen-depleted blood away from the retina (the…
Secondary Tumors
Cancer cells can spread through the bloodstream or the lymphatic system from…