Color vision deficiency (also called color blindness) is a vision disorder in which a person…
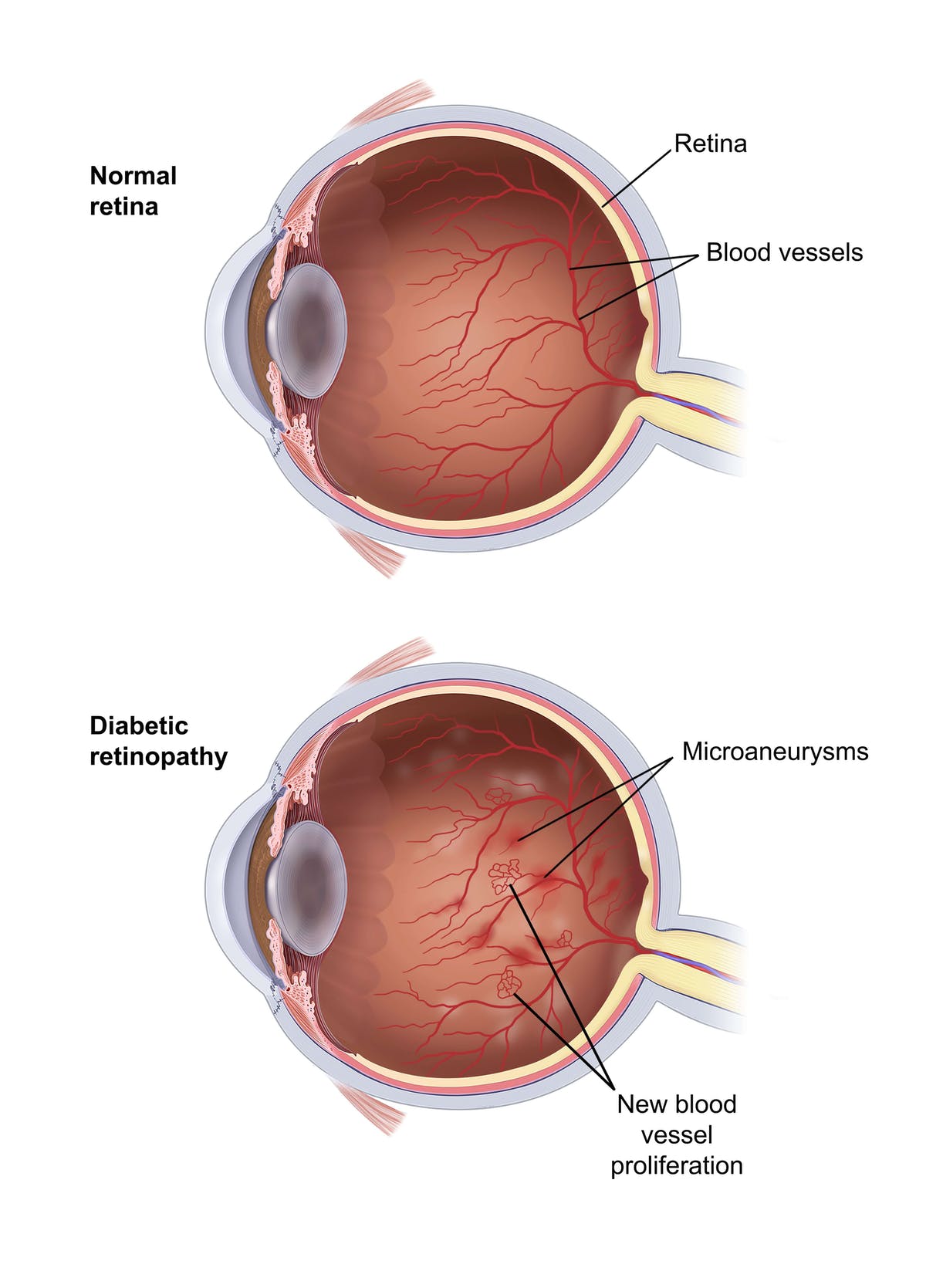
Diabetic retinopathy is an eye disorder in which changes in the blood vessels of the retina (the light-sensitive membrane that lines the back of the eye) can lead to vision loss or blindness. The disorder occurs in people who have diabetes, which can damage blood vessels, including those in the eye.
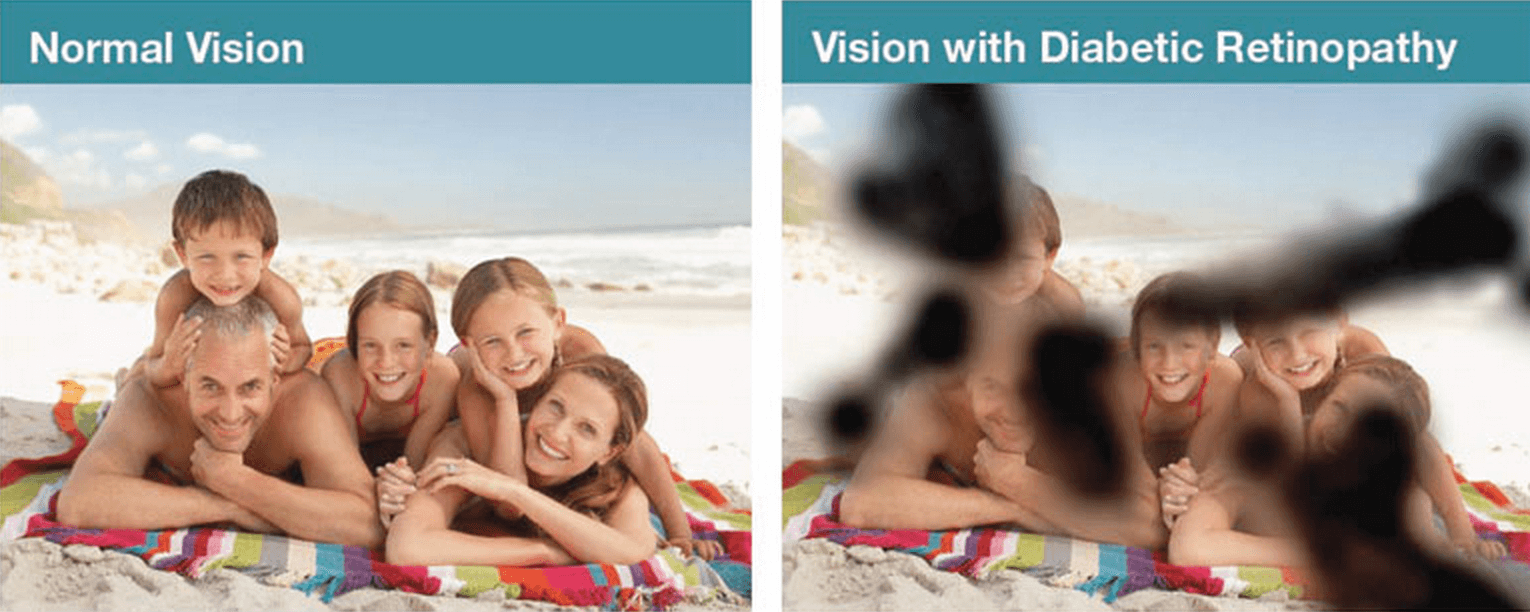
In some people who develop diabetic retinopathy, the blood vessels in the retina leak fluid. In others, abnormal new blood vessels grow on the surface of the retina and bleed and leak into the vitreous fluid (the substance that makes up the mass of the inside of the eyeball), preventing light from reaching the retina. The abnormal blood vessels also can produce scar tissue that pulls the retina away from the back of the eye, causing retinal detachment.
Anyone who has diabetes can develop diabetic retinopathy, and the longer you have diabetes, the more likely you are to develop this eye disorder. Nearly half of all people who have diabetes develop diabetic retinopathy. Good control of both blood sugar (glucose) levels and blood pressure and early detection and treatment of diabetic retinopathy can help slow progression of the disease and can help prevent vision loss and blindness.
Diabetic Retinopathy Treatments
To prevent diabetic retinopathy or to slow its progression, your doctor will recommend controlling the level of glucose in your blood with diet, exercise, and medication (insulin, in some cases). He or she will stress the importance of keeping your blood pressure within the normal range.
In some cases, an ophthalmologist may recommend laser surgery, in which a surgeon directs a highly concentrated beam of light onto the retina either to seal leaking blood vessels or to shrink abnormal blood vessels. The procedure is done using a local anesthetic and can be performed in the doctor’s office or in an outpatient facility; you return home the same day. Laser surgery can reduce the risk of severe vision loss from diabetic retinopathy, but it may not restore vision that has already been lost. After surgery you may lose some peripheral (side) vision, and your color and night vision may also be affected. In some cases, the surgery must be repeated.
For advanced cases of diabetic retinopathy in which leaking blood has filled the vitreous fluid, an ophthalmologist may recommend a type of microsurgery (delicate surgery performed under a microscope) called vitrectomy instead of laser surgery. In vitrectomy, the blood-filled vitreous fluid is removed and replaced with a clear saline (saltwater) solution. Other than improved vision, you will not notice any difference between the saline solution and the vitreous fluid. Vitrectomy may take several hours to complete and is performed in a hospital using either local or general anesthesia. You may need to stay in the hospital overnight. Recovery time varies depending on the extent of the problem.