Deep Vein Thrombosis Thrombosis is the formation of a blood clot (thrombus), which can partially…

Heart Attack
The heart needs a continuous supply of oxygen-rich blood from the coronary arteries to function properly. A heart attack occurs when a coronary artery is blocked, depriving part of the heart muscle of blood. The resulting damage to the heart muscle is the most common cause of death in people who have heart disease.
A blocked coronary artery usually results from long-term atherosclerosis, a condition in which arteries are narrowed by hardened fatty deposits called plaque. Most heart attacks occur when a plaque ruptures and a blood clot forms on the rough surface of the ruptured plaque and blocks blood flow through the artery suddenly and completely. In rare cases, a heart attack can result when a blood clot from another area of the heart breaks loose and blocks a coronary artery. Another rare cause of a heart attack is a spasm in a coronary artery that stops blood flow to the heart muscle. Using a stimulant drug such as cocaine can trigger this type of spasm.
Once a coronary artery has been blocked, damage to the heart muscle occurs quickly and can become permanent within minutes. In general, the longer the blockage lasts, the more extensive the damage to the heart muscle. Immediate medical treatment is essential to limit damage to the heart muscle and increase a person’s chances of survival.
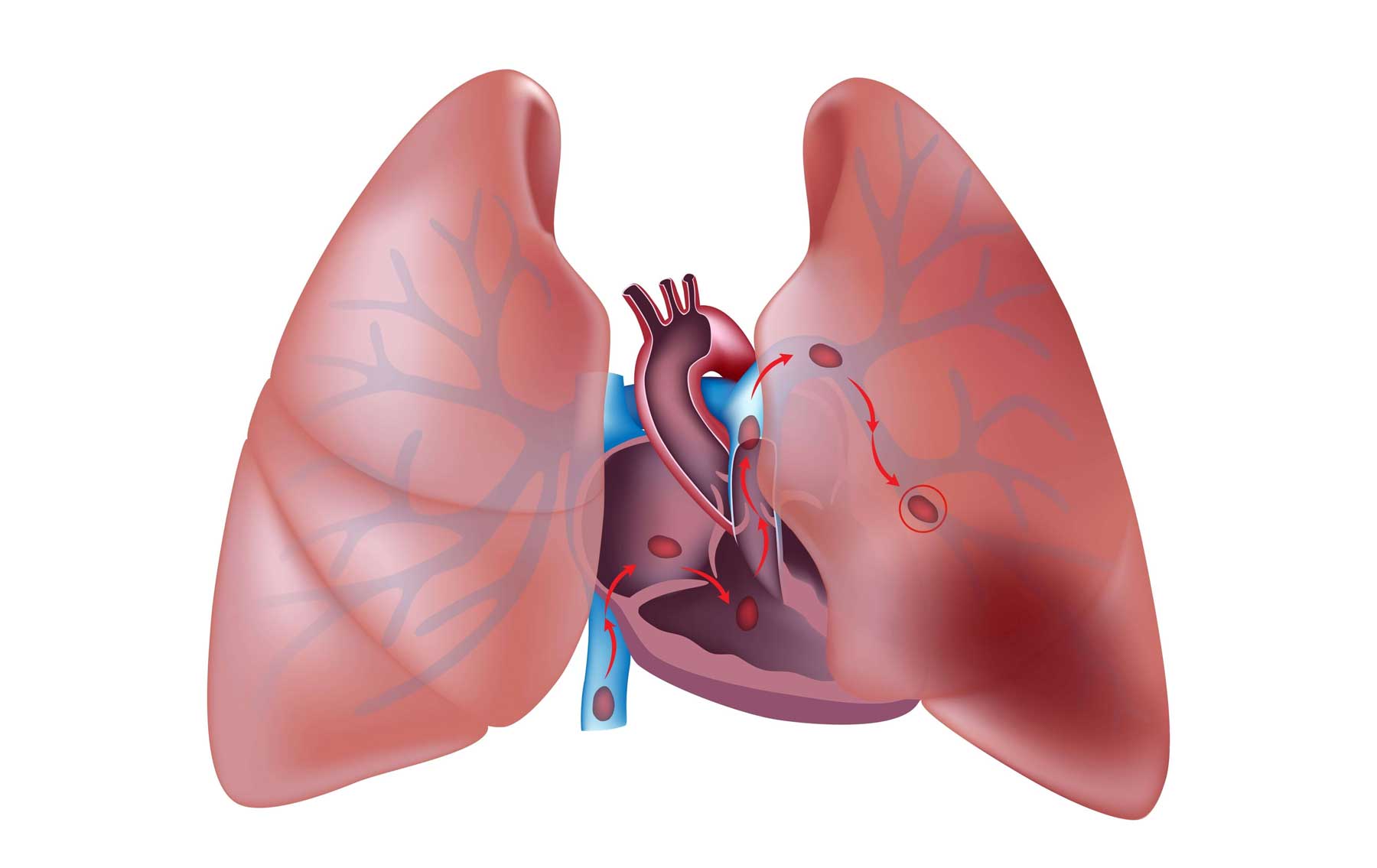
In some cases, after a heart attack, a blood clot may form inside one of the four chambers of the heart. If the clot breaks loose, it can travel through the bloodstream and cause damage to tissues elsewhere in the body. For example, if the clot blocks an artery that supplies blood to the brain, the result is a stroke. Sometimes damage caused by a heart attack weakens and stretches one of the walls of the heart chambers, causing a bulge in the wall called an aneurysm. An aneurysm can grow and burst without warning, causing uncontrolled bleeding (hemorrhage). Inactivity during bed rest may cause blood clots to form in the veins of the legs (deep vein thrombosis). These clots can break off, travel through the bloodstream, and block an artery that supplies blood to the lungs (pulmonary embolism).
Risk Factors
The following risk factors increase your chances of having a heart attack. While some of these can’t be changed—such as family health history, race, and gender—others can be modified or eliminated through lifestyle changes.
-
- Family health history. If siblings, parents, or grandparents had heart attacks at an early age, you are also at risk.
- Gender. Men are at greater risk of having a heart attack than women before age 55. After menopause, a woman’s risk is the same as a man’s.
- Undesirable cholesterol profile. An unhealthy cholesterol profile promotes atherosclerosis, which increases your risk of having a heart attack.
- High blood pressure. Uncontrolled high blood pressure promotes atherosclerosis.
- Smoking. Smoking (including exposure to secondhand smoke) raises blood pressure, damages artery walls, and increases the risk of blood clot formation.
- Diabetes. Uncontrolled diabetes promotes atherosclerosis and increases blood levels of LDL (harmful) cholesterol.
- Race. Blacks are at greater risk of having a heart attack than people of other races.
- Lack of exercise. A sedentary lifestyle often results in weight gain and a poor cholesterol profile.
- Being overweight. Weighing more than your ideal body weight increases your risk for high cholesterol, high blood pressure, and diabetes.
- Alcohol consumption. Drinking excessive amounts of alcohol can lead to high blood pressure and can raise blood levels of triglycerides (a potentially harmful type of fat in the blood).
- Stress. In some people, long-term stress can contribute to high blood pressure.
Symptoms
Symptoms of a heart attack vary in type and intensity from one person to another and from one heart attack to another in the same person. Some people may have a heart attack and have no symptoms. However, in most cases, the main symptom of a heart attack is sudden pain in the center of the chest. Some people describe the pain as a feeling of tightness, pressure, or fullness, or a squeezing sensation. The pain is usually severe and may spread to the back, left arm, neck, jaw, upper abdomen, and sometimes to the right arm. The pain may be continuous or may last for a few minutes, fade, and then return.
Most people who have a heart attack have recurring chest pain, shortness of breath, and fatigue for a few days before the attack. In some people, arrhythmia (irregular heartbeat) may also precede a heart attack. Unlike angina, the pain of a heart attack is not relieved with rest or after taking nitroglycerin (a medication prescribed to relieve angina). Also, heart attack pain is usually more severe and longer-lasting than angina.
Other common symptoms of a heart attack include dizziness, shortness of breath, sweating, chills, nausea, restlessness or anxiety, fainting, or weakness. Sometimes the lips, hands, or feet turn slightly blue. Women are more likely than men to have these symptoms in addition to chest pain. In rare cases, a heart attack does not cause symptoms and is detected by chance on an electrocardiogram (ECG), a recording of the electrical activity of the heart, performed for another purpose.
Some people may ignore their symptoms or assume they are caused by some other condition, such as indigestion or overexertion. However, because most deaths from a heart attack occur within an hour of the onset of symptoms, it is crucial to be able to recognize the symptoms and act quickly. The sooner treatment begins, the less damage to the heart muscle and the better the long-term prognosis.
Treatments
The sooner treatment for a heart attack begins, the better your chances of survival. Treatment may include medication, surgery, or both, depending on your overall health and the amount of damage to the heart muscle.
Medication
You may be given nitroglycerin to improve blood flow to and from your heart and to relieve pain. If your pain is severe, you may be given a strong pain reliever such as morphine. You will probably be given antiplatelet drugs (such as aspirin) or anticoagulant drugs (such as heparin) to help prevent blood clots from forming again in the coronary arteries or new clots from forming in the veins, especially in the legs. Beta blockers may be given to help reduce the heart’s workload by slowing the heartbeat and lowering blood pressure.
You may be given thrombolytic (clot-dissolving) drugs to dissolve the blood clot that is blocking the coronary artery. However, this treatment is effective only if no more than 6 hours have passed since the onset of symptoms. In most cases, thrombolytic drugs are given (usually by injection directly into a vein) as soon as the diagnosis of a heart attack is confirmed.
Surgery
You will have additional tests, such as a coronary angiogram, to determine whether the clot has dissolved and blood flow has been restored. If the tests show that the coronary artery is still blocked, a procedure such as angioplasty may be performed to reopen the artery. If the artery becomes blocked again after surgery, the procedure may be repeated a few days later.
As an alternative to treatment with a thrombolytic drug, your doctor may perform immediate angioplasty of the blocked blood vessel using specially designed instruments to remove the blood clot from the artery. Balloons and stents may be used to open the artery. In many cases, immediate angioplasty for a heart attack can be as effective as treatment with thrombolytic drugs in limiting the damage caused by a heart attack and improving a person’s chances of survival. In rare cases a doctor may perform emergency coronary artery bypass surgery at the time of a heart attack.
Preventing Another Heart Attack
If you have had a heart attack, you are at risk of having another. Treatment after a heart attack focuses on healing the heart and preventing another heart attack. The following steps can help you reduce your chances of having another heart attack:
-
- Have regular medical checkups to help ensure early detection and treatment of health problems.
- Keep your blood pressure under control and have your blood pressure checked as often as your doctor recommends.
- Have your blood cholesterol levels checked as often as your doctor recommends.
- Do not smoke or use other tobacco products.
- Maintain a healthy weight.
- Eat a low-fat diet that includes plenty of whole grains and fresh fruits and vegetables.
- Exercise regularly.
- Resume sexual activity when it is safe to do so (ask your doctor for advice).
- Manage your stress.
- Drink alcohol only in moderation.
- Take all medication exactly as prescribed.
- Before you leave the hospital, your doctor will refer you to a cardiac rehabilitation program designed to help you recondition your heart, lungs, and muscles, and improve your cholesterol profile. Cardiac rehabilitation begins in the hospital and continues for weeks or months after you return home. The program usually includes diet, exercise, and lifestyle counseling. You also may need to take medication that reduces strain on your heart, improves its efficiency, and prevents irregular heartbeats. Medications may include:
- Antiplatelet agents or anticoagulants
- Beta blockers
- Angiotensin-converting enzyme (ACE) inhibitors
- Cholesterol-lowering medications
- Calcium channel blockers