Meningiomas are the most common benign intracranial tumor. They originate from arachnoid cap cells, which are cells within the thin, spider web-like membrane that covers the brain and spinal cord. The arachnoid is one of three protective layers, collectively known as the meninges, surrounding the brain and the spinal cord. The meninges also include the dura mater and pia mater. Although the majority of meningiomas are benign, these tumors can grow slowly until they are very large if left undiscovered and, in some locations, can be severely disabling and life-threatening. Most patients develop a single meningioma; however, some patients may develop several tumors growing simultaneously in other parts of the brain or spinal cord.
Risk Factors
As noted earlier, meningiomas most often occur in people between the ages of 30 and 70. Children are not as likely as adults to develop meningioma.
Women are more than two times as likely as men to develop a meningioma. Malignant meningioma diagnoses are three times as likely in men. Spinal meningiomas occur 10 times more frequently in women than in men.
Exposure to ionizing radiation, especially high doses, has been associated with a higher incidence of intracranial tumors, particularly meningiomas. There also is evidence indicating a connection between meningiomas and low doses of radiation. The most well-known case involves children in Israel who were given radiation for scale ringworm between 1948 and 1960. Within the U.S., dental X-rays are the most common form of exposure to ionizing radiation. A number of studies have linked the number of full-mouth dental radiographs to increased risk of meningioma.
The genetic disorder Neurofibromatosis type 2 (NF2) is believed to put people at a higher risk of developing meningioma. Patients with NF2 also may be more likely to develop malignant or multiple meningiomas.
Treatments
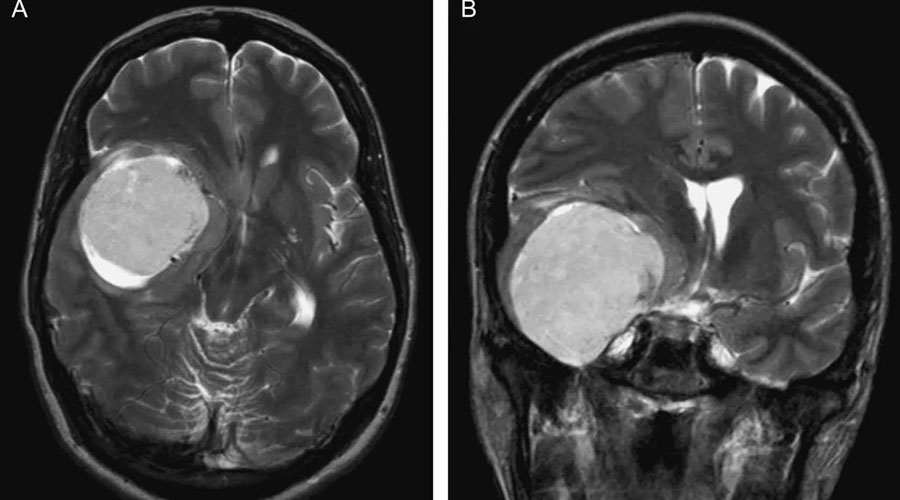
Surgery. Meningiomas primarily are benign tumors, frequently with defined borders and often enabling complete surgical removal, which offers the best chance for a cure. The neurosurgeon opens the skull through a craniotomy to enable full access to the meningioma. The goal of surgery is to remove the meningioma completely, including the fibers that attach it to the coverings of the brain and bone. However, complete removal can carry potential risks that may be significant, especially when the tumor has invaded brain tissue or surrounding veins.
Although the goal of surgery is to remove the tumor, the first priority is to preserve or improve the patient’s neurological functions. With patients for whom total removal of the tumor carries significant risk of morbidity (any side effect that can cause decreased quality of life), it may be better to leave some of the tumor in place and observe future growth with regular imaging studies. In such cases, the patient will be observed over a period of time with regular examinations and MRIs, while for other patients, radiation therapy may be deemed the best approach. It is common for patients to undergo preoperative embolization of the tumor to ensure safety during the surgical procedure. The embolization procedure is similar to a cerebral angiogram except that the surgeon fills the blood vessels in the tumor with glue to stop blood supply to the tumor.
Radiation Therapy. Radiation therapy uses high-energy X-rays to kill cancer cells and abnormal brain cells, and to shrink tumors. Radiation therapy may be an option if the tumor cannot be treated effectively through surgery.
Chemotherapy. Chemotherapy is rarely used to treat meningioma, except in atypical or malignant subtypes that cannot be adequately treated with surgery and/or radiation therapy.