A spinal tumor is an abnormal mass of tissue within or surrounding the cord and/or spinal column. These cells…
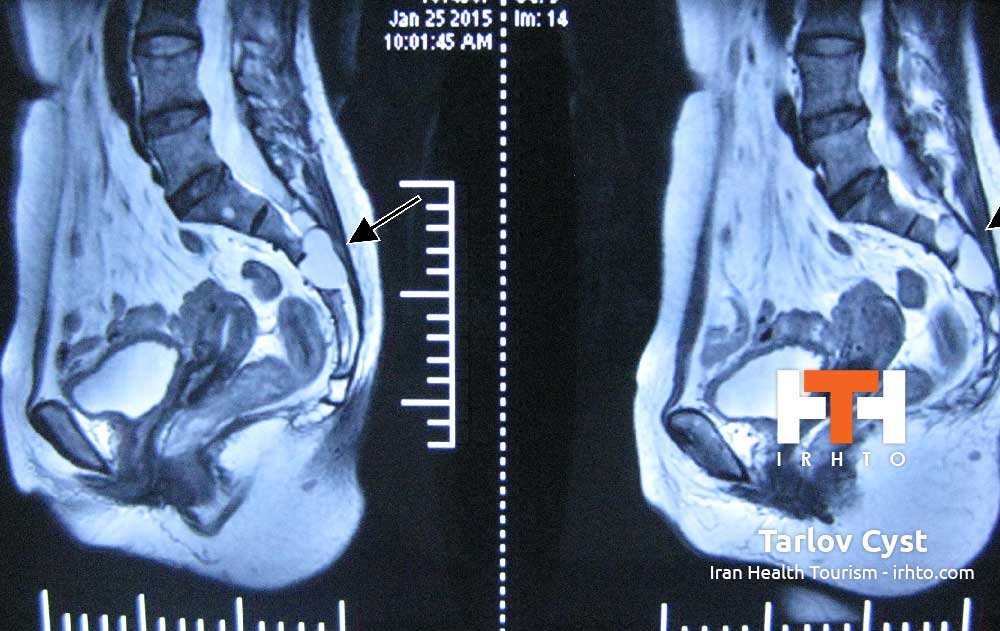
Tarlov cysts are fluid-filled nerve root cysts found most commonly at the sacral level of the spine – the vertebrae at the base of the spine. These cysts typically occur along the posterior nerve roots. Cysts can be valved or nonvalved. The main feature that distinguishes Tarlov cysts from other spinal lesions is the presence of spinal nerve root fibers within the cyst wall or in the cyst cavity itself.
Due to the close proximity to the lower pelvic region, patients may be misdiagnosed with herniated lumbar discs, arachnoiditis and in females, gynecological conditions. An accurate diagnosis may be further complicated if the patient has another condition that affects the same region.
Causes [h4]
Although the exact cause is unknown, there are theories as to what may cause an asymptomatic Tarlov cyst to produce symptoms. In several documented cases, accidents or falls involving the tailbone area of the spine caused previously undiagnosed Tarlov cysts to flare up.
Treatments [h4]
Nonsurgical Treatment. Nonsurgical therapies include lumbar drainage of the cerebrospinal fluid (CSF), CT scanning-guided cyst aspiration and a newer technique involving removing the CSF from inside the cyst and then filling the space with a fibrin glue injection. Unfortunately, none of these procedures prevent symptomatic cyst recurrence.
Surgery. Tarlov cyst surgery involves exposing the region of the spine where the cyst is located. The cyst is opened and the fluid drained, and then in order to prevent the fluid from returning, the cyst is occluded with a fibrin glue injection or other matter.
Neurosurgical techniques for symptomatic Tarlov cysts include simple decompressive laminectomy, cyst and/or nerve root excision and microsurgical cyst fenestration and imbrication.
The authors of one study found that patients with Tarlov cysts larger than 1.5 cm and with associated radicular pain or bowel/bladder dysfunction benefited most from surgery. The benefits of surgery should always be weighed carefully against its risks.
Vertebral Compression Fractures [h3]
Vertebral compression fractures (VCFs) are the most common fracture in patients with osteoporosis, affecting about 750,000 people annually. VCFs affect an estimated 25 percent of all postmenopausal women in the U.S. The prevalence of this condition steadily increases as people age, with an estimated 40 percent of women age 80 and older affected. Although far more common in women, VCFs are also a major health concern for older men.
People who have sustained one osteoporotic VCF are at five times the risk of sustaining a second VCF. Occasionally, a VCF can be present with either minor symptoms or no symptoms, but the risk still exists for additional VCFs to occur.
Causes [h4]
VCFs occur when the bony block or vertebral body in the spine collapses, which can lead to severe pain, deformity and loss of height. These fractures more commonly occur in the thoracic spine (the middle portion of the spine), especially in the lower part. While osteoporosis is the most common cause, these fractures may also be caused by trauma or metastatic tumors.
In people with severe osteoporosis, a VCF may be caused by simple daily activities, such as stepping out of the shower, sneezing vigorously or lifting a light object. In people with moderate osteoporosis, it usually takes increased force or trauma, such as falling down or attempting to lift a heavy object to cause a VCF. People with healthy spines most commonly suffer a VCF through severe trauma, such as a car accident, sports injury or a hard fall.
Metastatic tumors should be considered as the cause in patients younger than 55 with no history of trauma or only minimal trauma. The bones of the spine are a common place for many types of cancers to spread. The cancer may cause destruction of part of the vertebra, weakening the bone until it collapses.
Treatments [h4]
Nonsurgical Treatment [h5]
Traditionally, people with severe pain from VCFs have been treated with bed rest, medications, bracing or invasive spinal surgery, often with limited effectiveness. Pain secondary to acute vertebral fracture appears to be caused in part by vertebral instability (nonunion or slow-forming union) at the fracture site. VCF-related pain that is allowed to heal naturally can last as long as three months. However, the pain usually decreases significantly in a matter of days or weeks.
Bed rest may be advised for a short period of time, followed by a limitation on some activities. However, prolonged inactivity should be avoided.
Over-the-counter pain medications are often effective in relieving pain. Both acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly recommended. Narcotic pain medications and muscle relaxants are often prescribed but only for short periods of time, due to the risk of addiction.
Back bracing can provide external support to limit the motion of fractured vertebrae, similar to the support a cast provides on a leg fracture. The rigid style of back brace limits spine-related motion greatly, which may help reduce pain.
While immediate treatment is essential to alleviating the pain and risks of the fracture, prevention of subsequent fractures is very important. Your physician may prescribe bone-strengthening drugs known as bisphosphonates (i.e.: Actonel, Boniva and Fosamax) to help stabilize or restore bone loss.
When conservative treatment options have proven ineffective, two minimally invasive procedures, called vertebroplasty and kyphoplasty, may be considered as treatment options. Recent advances in spinal procedures have reduced the need for invasive surgery in many cases.
Vertebroplasty and Kyphoplasty [h5]
Vertebroplasty for the treatment of VCFs was introduced in the U.S. in the early 1990s. The procedure is usually done on an outpatient basis, although some patients stay in the hospital overnight. Vertebroplasty takes from one to two hours to perform, depending on the number of vertebrae being treated. The procedure may be performed with a local anesthetic and intravenous sedation or general anesthesia. Using x-ray guidance, a small needle containing specially formulated acrylic bone cement is injected into the collapsed vertebra. The cement hardens within minutes, strengthening and stabilizing the fractured vertebra. Most experts believe that pain relief is achieved through mechanical support and stability provided by the bone cement.
A newer procedure, called kyphoplasty, involves an added procedure performed before the cement is injected into the vertebra. First, two small incisions are made and a probe is placed into the vertebral space where the fracture is located. The bone is drilled and one balloon (called a bone tamp) is inserted on each side. The two balloons are then inflated with contrast medium (which are visualized using image guidance x-rays) until they expand to the desired height and removed. The spaces created by the balloons are then filled with the cement. Kyphoplasty has the added benefit of restoring height to the spine.



