Cerebral Aneurysm A cerebral or intracranial aneurysm is an abnormal focal dilation of an artery in the…
Stroke
Stroke is an abrupt interruption of constant blood flow to the brain that causes loss of neurological function. The interruption of blood flow can be caused by a blockage, leading to the more common ischemic stroke, or by bleeding in the brain, leading to the more deadly hemorrhagic stroke. Ischemic stroke constitutes an estimated 87 percent of all stroke cases. Stroke often occurs with little or no warning, and the results can be devastating.
It is crucial that proper blood flow and oxygen be restored to the brain as soon as possible. Without oxygen and important nutrients, the affected brain cells are either damaged or die within a few minutes. Once brain cells die, they generally do not regenerate and devastating damage may occur, sometimes resulting in physical, cognitive and mental disabilities.
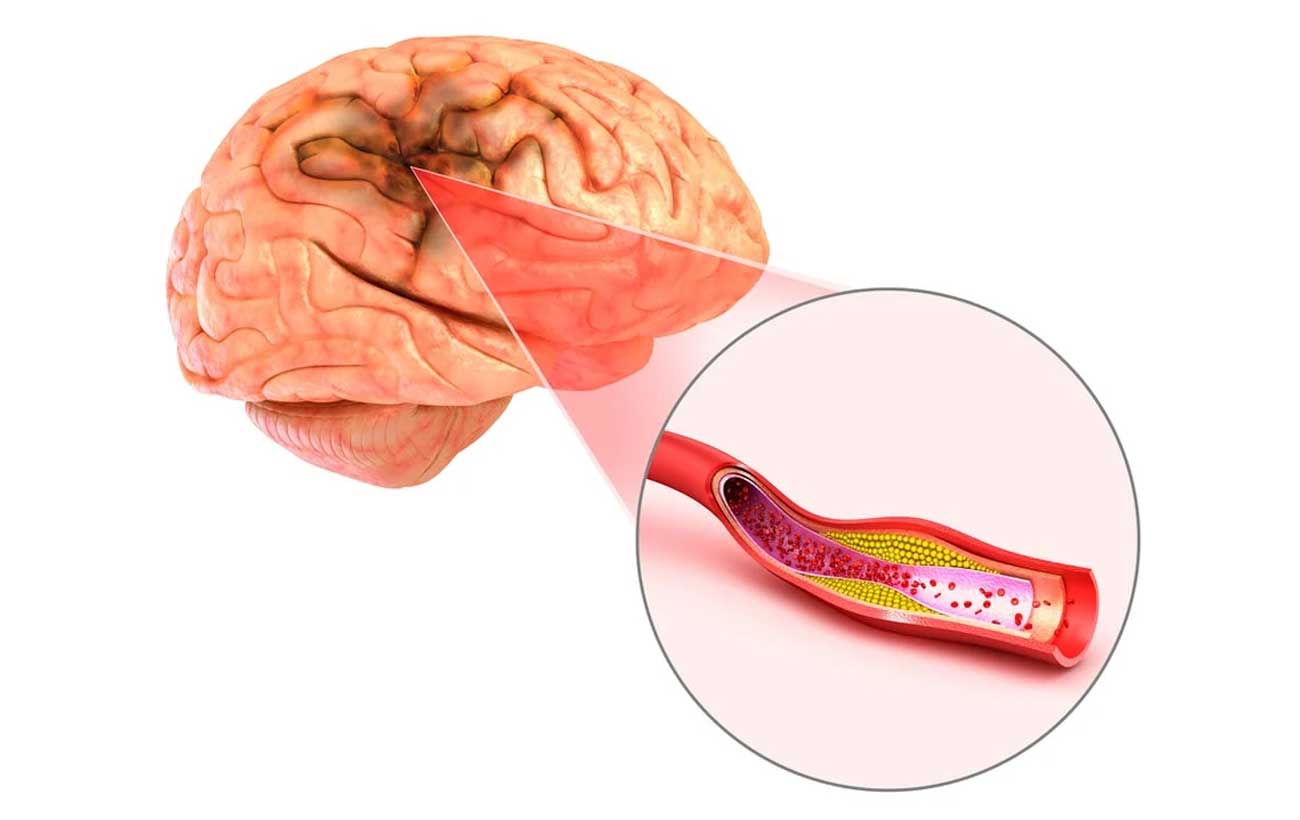
Ischemic Stroke
- Thrombotic (cerebral thrombosis) is the most common type of ischemic stroke. A blood clot forms inside a diseased or damaged artery in the brain resulting from atherosclerosis (cholesterol-containing deposits called plaque), blocking blood flow.
- Embolic (cerebral embolism) is caused when a clot or a small piece of plaque formed in one of the arteries leading to the brain or in the heart, is pushed through the bloodstream and lodges in narrower brain arteries. The blood supply is cut off from the brain due to the clogged vessel.
Transient ischemic attack (TIA)
This is a warning sign of a possible future stroke and is treated as a neurological emergency. Common temporary symptoms include difficulty speaking or understanding others, loss or blurring of vision in one eye and loss of strength or numbness in an arm or leg. Usually these symptoms resolve in less than 10 to 20 minutes and almost always within one hour. Even if all the symptoms resolve, it is very important that anyone experiencing these symptoms call 911 and immediately be evaluated by a qualified physician.
Hemorrhagic Stroke
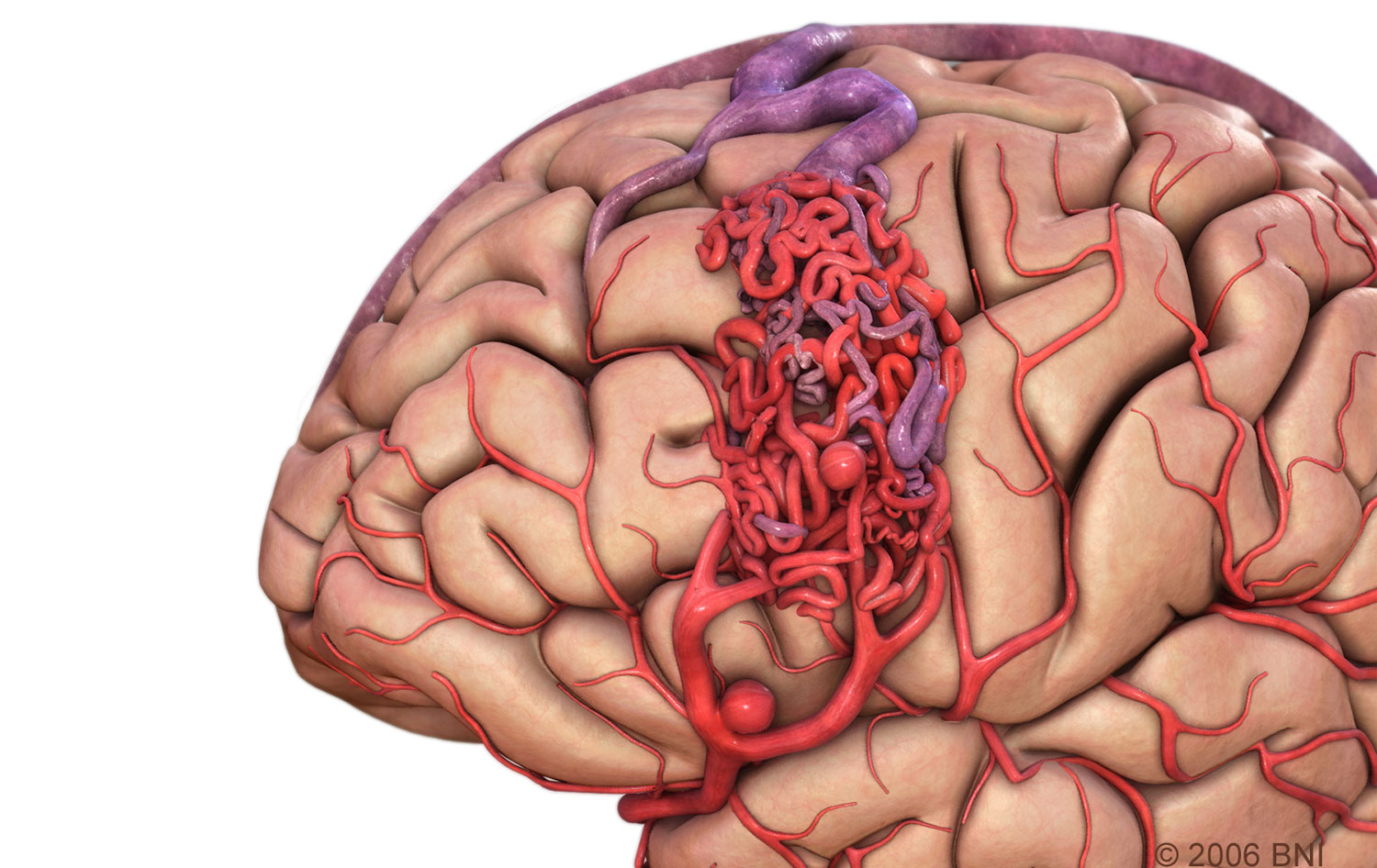
- Subarachnoid Hemorrhage is bleeding that occurs in the space between the surface of the brain and skull. A common cause of subarachnoid hemorrhagic stroke is a ruptured cerebral aneurysm, an area where a blood vessel in the brain weakens, resulting in a bulging or ballooning out of part of the vessel wall; or the rupture of an arteriovenous malformation (AVM), a tangle of abnormal and poorly formed blood vessels (arteries and veins), with an innate propensity to bleed.
- Intracerebral Hemorrhage is bleeding that occurs within the brain tissue. Many intracerebral hemorrhages are due to changes in the arteries caused by long-term hypertension. Other potential causes may be delineated through testing.
Risk Factors
Although they are more common in older adults, strokes can occur at any age. Understanding the factors that increase your risk of a stroke and recognizing the symptoms may help you prevent a stroke. Receiving early diagnosis and treatment may improve your chances for complete recovery.
Controllable or treatable risk factors for stroke include:
- Smoking: You can decrease your risk by quitting smoking. Your risk may be increased further if you use some forms of oral contraceptives and are a smoker. There is recent evidence that long-term secondhand smoke exposure may increase your risk of stroke.
- High blood pressure: Blood pressure of 140/90 mm Hg or higher is the most important risk factor for stroke. It usually has no specific symptoms and no early warning signs. That is why it is important to have your blood pressure checked regularly. Controlling your blood pressure is crucial to stroke prevention.
- Carotid or other artery disease: The carotid arteries in your neck supply blood to your brain. A carotid artery narrowed by fatty deposits from atherosclerosis may become blocked by a blood clot. Carotid arteries are treated by neurosurgeons through carotid endarterectomy, a procedure in which an incision is made in the neck and plaque is removed from the artery; or carotid artery angioplasty and stenting, an endovascular procedure that requires no surgical incision in the neck.
- History of TIAs (Transient ischemic attack): About 30 percent of strokes are preceded by one or more TIAs that can occur days, weeks or even months before a stroke.
- Diabetes: It is crucial to control your blood sugar levels, blood pressure and cholesterol levels. Diabetes, especially when untreated, puts you at greater risk of stroke and has many other serious health implications.
- High blood cholesterol: A high level of total cholesterol in the blood (240 mg/dL or higher) is a major risk factor for heart disease, which raises your risk of stroke. Recent studies show that high levels of LDL (bad) cholesterol (greater than 100 mg/dL) and triglycerides (blood fats, 150 mg/dL or higher) increase the risk of stroke in people with previous coronary heart disease, ischemic stroke or TIAs. Low levels (less than 40 mg/dL) of HDL (good) cholesterol also may increase stroke risk. You can often improve your cholesterol levels by decreasing the salt and saturated fat in your diet. However, some people inherit genes associated with elevated levels of cholesterol. Although they may eat well and exercise, they still may have high cholesterol and must take medication to control it.
- Physical inactivity and obesity: Being inactive, obese or both can increase your risk of high blood pressure, high blood cholesterol, diabetes, heart disease and stroke. Getting 30 minutes of moderate exercise, five days a week can help reduce your risk of stroke. Check with your doctor first before starting any exercise program if you have any health problems or have been inactive.
- Recent research shows evidence that people receiving hormone replacement therapy (HRT) have an overall 29 percent increased risk of stroke, in particular ischemic stroke.
Uncontrollable risk factors include:
- Age: People of all ages, including children, have strokes. But the older you are, the greater your risk of stroke.
- Gender: Stroke is more common in men than in women. In most age groups, more men than women will have a stroke in a given year. However, women account for more than half of all stroke deaths. Women who are pregnant have a higher stroke risk. Some research has indicated that women may experience and interpret stroke symptoms differently than men, causing them to delay seeking medical care and contributing to their higher stroke mortality rates.
- Heredity and race: You have a greater risk of stroke if a parent, grandparent, sister or brother has had a stroke. African Americans have more than two times the risk of stroke compared to Caucasians, partly related to the prevalence of hypertension. Hispanics also have an elevated stroke risk.
- Prior stroke or heart attack: If you have had a stroke, you are at much higher risk of having another one. If you have had a heart attack, you are also at higher risk of having a stroke.
Treatments
Ischemic Stroke Treatment
Ischemic stroke is treated by removing obstruction and restoring blood flow to the brain. The only U. S. Food and Drug Administration (FDA)-approved medication for ischemic stroke is tissue plasminogen activator (tPA), which must be administered within a three-hour window from the onset of symptoms to work best. Unfortunately, only 3- 5 percent of those who suffer a stroke reach the hospital in time to be considered for this treatment, and the actual use of tPA is considerably lower. This medication carries a risk for increased intracranial hemorrhage and is not used for hemorrhagic stroke.
Emergency Surgical Stroke Treatment: Neurointerventional Procedures
Microcatheter-based surgical interventions for stroke may include the use of a small microcatheter, delivered through a larger guiding catheter inserted at the groin through a small incision. A micro guidewire is used to navigate the microcatheter to the site of obstruction in the brain. Thrombolytic medication, such as tPA, can then be administered directly to the occluding thrombus. This kind of treatment, which delivers thrombolytic medication intraarterially, is more specific than IV (intravenous) tPA and consequently may require significantly lesser dosages of medication. The time limit to implement this type of intervention is also significantly (double) longer than that for IV TPA. Generally, only Comprehensive Stroke Care Centers offer this type of treatment.
Clot Retrieval Devices
The Merci Retriever, approved in 2004 by the FDA, is a corkscrew- shaped device used to help remove blood clots from the arteries of stroke patients. A small incision is made in the patient’s groin, into which a small catheter is fed until it reaches the arteries in the neck. At the neck, a small catheter inside the larger catheter is guided through the arteries into the brain, until it reaches the brain clot. A straight wire inside the small catheter pokes out beyond the clot and automatically coils into a corkscrew shape. It is pulled back into the clot, the corkscrew spinning and grabbing the clot. A balloon inflates in the neck artery, cutting off blood flow, so the device can pull the clot out of the brain safely. The clot is removed through the catheter with a syringe.
Penumbra is also a microcatheter-based system device, which works by an aspiration principle. It was approved by the FDA in 2008.
Stentriever devices are the newest generation of embolectomy devices for stroke. They are still in an investigative phase but work by breaking up the occluding clot, combined with aspiration or withdrawal.
Hemorrhagic Stroke Treatment
Hemorrhagic stroke usually requires surgery to relieve intracranial (within the skull) pressure caused by bleeding. Surgical treatment for hemorrhagic stroke caused by an aneurysm or defective blood vessel can prevent additional strokes. Surgery may be performed to seal off the defective blood vessel and redirect blood flow to other vessels that supply blood to the same region of the brain.
For a patient with a ruptured cerebral aneurysm, surgical elimination of the aneurysm is only the beginning. Intensive care recovery for the next 10-14 days is the rule, during which time a multitude of complications related to subarachnoid hemorrhage (SAH) can and do occur. At some time during that period (often immediately upon completion of surgery), cerebral angiography or a substitute study is done to document that the aneurysm has been eliminated. The first two to five days after SAH represent the greatest threat of brain swelling; at which time special measures (both medical and surgical) are used to diminish the effect of swelling on intracranial pressure. Near the end of this initial period, the risk period for delayed cerebral vasospasm begins and lasts the better part of the next 14 days. Intercurrent infections such as pneumonia are common, and hydrocephalus may develop.
Surgery/Clipping
Prior to surgery, the exact location of the subarachnoid hemorrhage or aneursym is identified through cerebral angiography images. An operation to “clip” the aneurysm is performed by doing a craniotomy (opening the skull surgically) and isolating the aneurysm from the normal bloodstream. In addition, a craniectomy, a surgical procedure in which part of the skull is removed and left off temporarily, may be done to help relieve increased intracranial pressure.
One or more tiny titanium clips with spring mechanisms are applied to the base of the aneurysm, allowing it to deflate. The size and shape of the clips is selected based on the size and location of the aneurysm. Clips are permanent, remain in place and generally provide a durable cure for the patient. Angiography is used to confirm exclusion of the aneurysm from the cerebral circulation and the preservation of normal flow of blood in the brain.
Endovascular (Neurointerventional) Treatment
Neurointerventional procedures for cerebral aneurysm share the advantages of no incision made in the skull and an anesthesia time that is often dramatically shorter than for craniotomy and microsurgical clipping.
In endovascular micro coil embolization, a needle is placed into the femoral artery of the leg, and a small catheter is inserted. Utilizing x-ray guidance, the catheter is advanced through the body’s arterial system to one of the four blood vessels that feed the brain. A smaller microcatheter is fed into the aneurysm, and once properly positioned, a thin wire filament or “coil” is advanced into the aneurysm. The flexible, platinum coil is designed to conform to the shape of the aneurysm. Additional coils are advanced into the aneurysm to close the aneurysm from the inside. This prevents flow of blood into the aneurysm by causing a clot to form on the inside.
Balloon-assisted coiling uses a tiny balloon catheter to help hold the coil in place. Although this has been shown in several studies to increase risks, ongoing innovations in this relatively new technology has helped improve its efficacy. Combination stent and coiling utilizes a small flexible cylindrical mesh tube that provides a scaffold for the coiling. Intracranial stenting and other innovations are quite new, and endovascular technology is in a constant state of development. These adjuncts allow coiling to be considered for cerebral aneurysms that may not have an ideal shape for conventional coiling.
Stroke Rehabilitation
Recovery and rehabilitation are among the most important aspects of stroke treatment. As a rule, most strokes are associated with some recovery, the extent of which is variable. In some cases, undamaged areas of the brain may be able to perform functions that were lost when the stroke occurred. Rehabilitation includes physical therapy, speech therapy and occupational therapy. This type of recovery is measured in months to years.
- Physical therapy involves using exercise and other physical means (e.g., massage, heat) and may help patients regain the use of their arms and legs and prevent muscle stiffness in patients with permanent paralysis.
- Speech therapy may help patients regain the ability to speak.
- Occupational therapy may help patients regain independent function and relearn basic skills (e.g., getting dressed, preparing a meal and bathing).